
About our Child and Adolescent Psychiatry Project
The Child and Adolescent Psychiatry Project began in 2018. It aims to create sustainable improvement in mental health and full inclusion in community life for children with psycho-social disabilities (CPSD).
High numbers of children with psycho-social disabilities experience barriers to integrating into family and community life. The barriers are due to the stigma attached to psycho-social disabilities, a lack of infrastructure, and community members lacking awareness about children with psycho-social disabilities.
We provide training for family and community members, as well as access to mobile clinics and information on services available. In doing so, we aim to ensure children with psycho-social disability will receive more support from their families and communities. They will also have increased access to appropriate services. Our hope is that this increased support will lead to an improvement in their functional mental health, as well as increased inclusion into their schools and community life.
We also provide training for health professionals; develop materials to help the integration of children with psycho-social disabilities; advocate for policy changes that will support further integration of CPSDs into their schools and communities; and work with other NGOs and government workers in the area to help children with psycho-social disabilities integrate.
Curious about our work in Mental Health? Read more here.
Our Work in Community Based Mental Health
Our Community Based Mental Health Project began in 2018. Its aim is the sustainable improvement in the lives of People with Psychosocial Disabilities (PPSD) and their families. We aim to achieve this through integrated social, psychological and medical care and increased social inclusion. We want to reduce the barriers for people with psycho social disorders, so that they can receive the care they need; care at family, community, primary and secondary health care levels.
Many people with pyscho-social disorders do not receive the services and support they need. This is primarily due to the stigma surrounding pyscho-social disorders; a lack of awareness; lack of accurate research on the situation in Afghanistan; and a lack of resources.
Our Strategy
By focusing on engaging at the community level, the Community Based Mental Health Project helps to develop community capacity for supporting people with pyscho-social disorders. We are able to connect PPSD and communities with the resources and support services that are available.
Instead of focusing solely on medical help, this project provides a holistic approach to support. While we help to refer people with psycho-social disabilities to the appropriate medical and counselling services, we also spend time with all levels of the community. In doing so, we can help address the stigma and social issues of PPSD, and also address accessibility issues and provide education for those surrounding people with pyscho-social disorders.
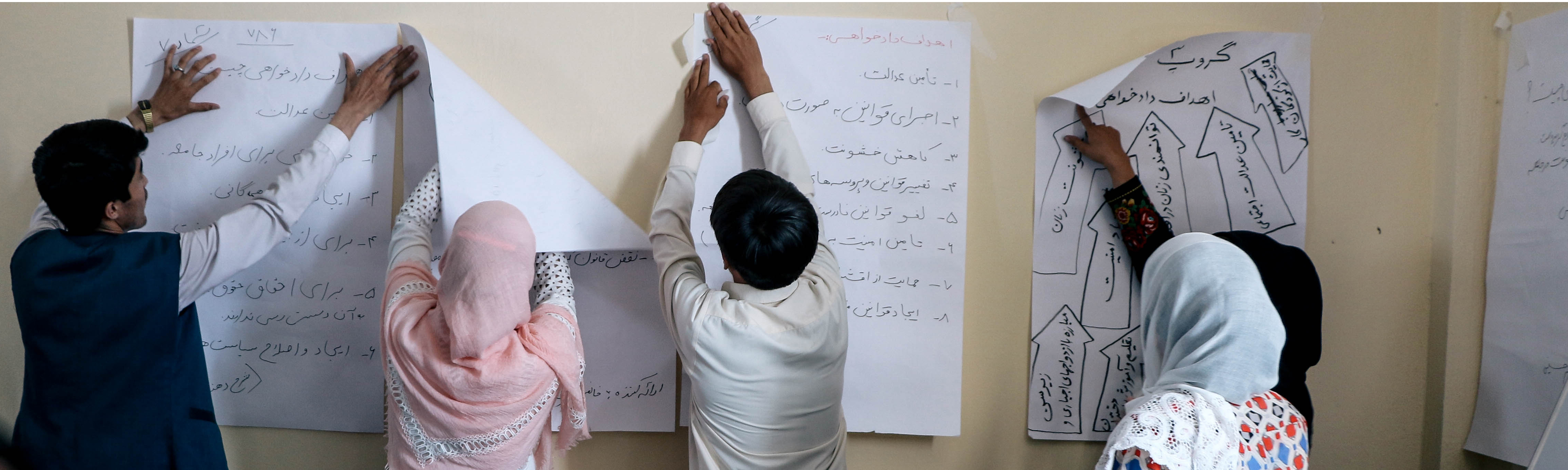
We provide training for family and community members on how to support people with pyscho-social disorders; we also include community leaders, religious leaders, and health care professionals in training. This training includes information on awareness and advocacy for community and religious leaders and health care professionals. We help communities to establish support groups, refer PPSD to services when needed and help families to support them in receiving home or centre-based service, and build awareness through television programmes as well.
Want to learn more?
Stay posted for more information on our Community Based Mental Health Project. If you would like to learn more about our work in Mental Health in general, click here.
Posts about Mental Health Programme 28
After years of domestic violence and physical abuse at the hand of her husband, who struggled with addition, Rita* was experiencing headaches, insomnia, feelings of aggression, restlessness, and interpersonal conflict. […]

This year, for the first time ever, the people of Kandahar and Farah provinces – which have a combined population of over two million – will have access to two psychiatrists, who recently graduated from IAM’s Mental Health Programme in 2020. These psychiatrists will begin providing mental health services in hospitals and other units, which means people with mental health problems in these areas will have access to the help they need.
Seven years of depression. Four months of counselling. A family transformed. “Now, our life is ten times better than before” Sabera* would beat her children and pull out chunks of […]






